Screening and Genetic Testing in Melanoma
*Please note: This slide show is not intended to be a substitute for professional medical advice. Always consult your doctor about any questions you may have regarding a medical condition.
Melanoma and your genes
Melanoma, like all cancers, is caused by changes in genes. Understanding the genetic changes that lead to melanoma can help with finding the best treatment for each patient.
Melanoma occurs most often in the skin. Less often, it can occur in the eye or elsewhere, such as the mouth or throat. This slide show focuses on genetic changes that lead to melanoma in the skin.
How does cancer start?
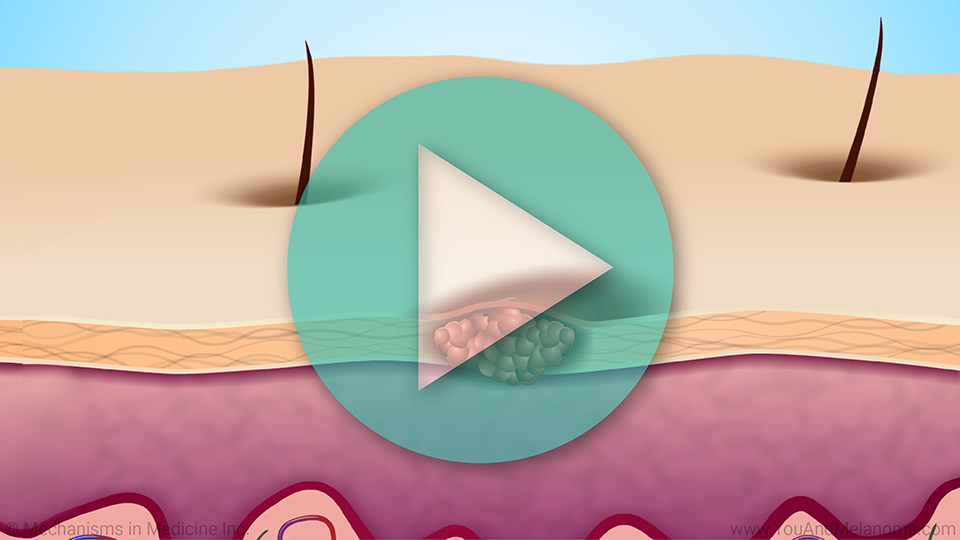
Cancer occurs when cells in the body start to grow and divide uncontrollably. It starts with a change in a single gene within a cell.
Genes are made of DNA, the basic genetic material of life. Genes can change in two ways.
How does cancer start? – Mutations in the sequence of DNA
First, a change, or mutation, can occur in the sequence of DNA building blocks that make up a gene.
Mutations are common. Most of them don't cause cancer. The body corrects most mutations.
Usually, a single mutation will not cause cancer. Cancer usually occurs due to a buildup of mutations over many years.
How does cancer start? – Mutations in the sequence of DNA
Most mutations are caused by damage to genes that happens during a person's life. These are the most common cause of cancer.
In rare cases, mutations are passed from a parent to a child. These mutations can cause cancer to run in families.
How does cancer start? – Epigenetic changes
The second way genes can change is that a gene's functioning changes without changing the sequence of DNA building blocks.
This type of change may cause the gene to be underactivated, overactivated, or "turned off". Or, all or part of the gene may be missing.
Genes that play a special role in cancer
Some genes play a special role in cancer.
-
Oncogenes promote cancer by helping cells stay alive, grow, and divide. They are often found at abnormally high levels in tumor cells.
-
Tumor suppressor genes keep cancer from developing by:
- Controlling cell growth
- Helping the body get rid of abnormal cells
- Fixing mistakes in DNA
Genes that play a special role in cancer
Cancer can start to grow when genetic changes occur that:
-
Keep oncogenes turned on
- Turn off tumor suppressor genes
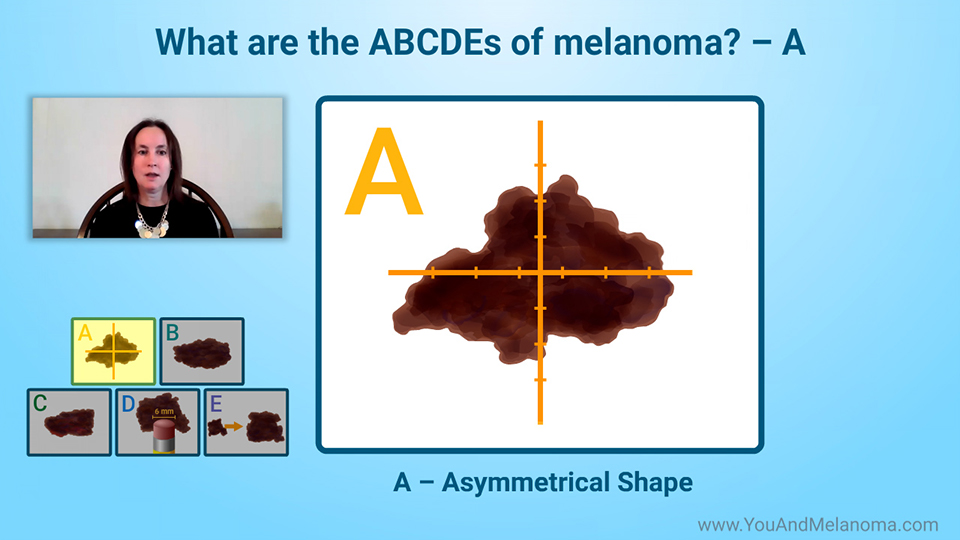
How does melanoma start? Overexposure to UV rays
Melanoma in the skin starts when certain skin cells change and start to grow and divide uncontrollably.
Overexposure to ultraviolet or UV rays is the most common cause of genetic changes that lead to melanoma in the skin.
How does melanoma start? UV rays can damage genes in skin cells
Most UV rays come from sunlight. They may also come from tanning beds. Tanned skin is a sign of damage to skin cells.
UV rays can damage the genes in skin cells. These changes may occur over many years before they turn into melanoma. People who have many spots, or moles, on their skin are at higher risk for melanoma.
Genetic mutations and non-inherited melanoma
The most common mutation in non-inherited melanoma is in an oncogene called BRAF. Around half of all people diagnosed with melanoma have a BRAF mutation. However, not all moles with BRAF mutations will become melanoma.
Another common mutation is in an oncogene gene called NRAS. About one in five people diagnosed with melanoma has an NRAS mutation.
Several other genetic mutations may also be found in people with melanoma.
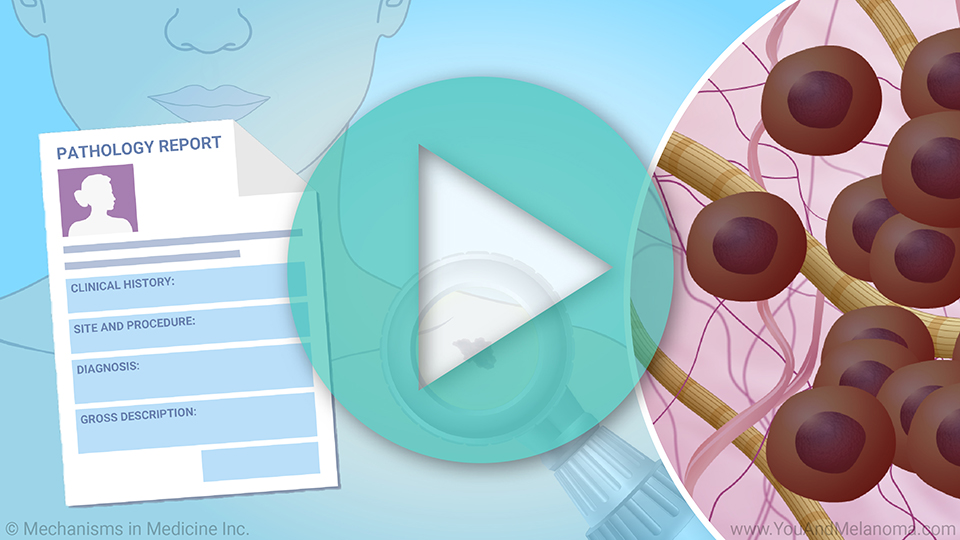
Genetic mutations and early diagnosis of melanoma
Melanoma treatment has the best chance of success when the disease is diagnosed at a very early stage.
A pigmented lesion assay (PLA) adhesion patch test is now available that can diagnose very early-stage melanoma genes in the skin. It does this in two ways:
- It looks for mutations in a gene called TERT
- It measures the levels of two genes, called LINC and PRAME, that are found in melanoma but not in normal skin
Genetic mutations and inherited melanoma
In about one in ten cases, melanoma occurs in multiple members of the same family.
Genetic mutations and inherited melanoma
People with inherited melanoma often have changes in a tumor suppressor gene called CDKN2A. About four in ten families affected by inherited melanoma have mutations in this gene.
People with this mutation are more likely to be diagnosed with melanoma, often at an early age. They should have regular skin exams to detect melanoma as early as possible.
Should I get genetic testing to determine my risk for melanoma?
A doctor may recommend genetic testing to determine your risk for melanoma if:
-
You have had three or more melanomas that have grown deeper into the skin, including one that was diagnosed before age 45
-
You have three or more close relatives who have had melanoma or cancer of the pancreas
-
You have certain unusual-looking moles
Should I get genetic testing to determine my risk for melanoma?
Talk with your doctor about whether genetic testing to determine your risk for melanoma is right for you.
References
- American Academy of Dermatology. Should I get genetic testing for melanoma? https://www.aad.org/public/diseases/skin-cancer/types/common/melanoma/genetic-testing
- American Cancer Society. Targeted Therapy Drugs for Melanoma Skin Cancer. Last revised August 2019. https://www.cancer.org/cancer/melanoma-skin-cancer/treating/targeted-therapy.html
- American Cancer Society. Oncogenes and tumor suppressor genes. Last revised June 2014. https://www.cancer.org/cancer/cancer-causes/genetics/genes-and-cancer/oncogenes-tumor-suppressor-genes.html
- American Cancer Society. What Causes Melanoma Skin Cancer? Last revised August 14, 2019. https://www.cancer.org/cancer/melanoma-skin-cancer/causes-risks-prevention/what-causes.html
- Cancer.Net. Melanoma: Risk Factors and Prevention. August 2020. https://www.cancer.net/cancer-types/melanoma/risk-factors-and-prevention
- Cancer.Net. Familial Malignant Melanoma. April 2020. https://www.cancer.net/cancer-types/familial-malignant-melanoma
- Cancer.Net. The Genetics of Cancer. March 2018. https://www.cancer.net/navigating-cancer-care/cancer-basics/genetics/genetics-cancer
- Medline Plus. CDKN2A gene. Last updated August 18, 2020. https://medlineplus.gov/genetics/gene/cdkn2a/#conditions
- MedlinePlus. What is epigenetics? Last updated May 3, 2021. https://medlineplus.gov/genetics/understanding/howgeneswork/epigenome/
- Melanoma Research Foundation. Cutaneous Melanoma. Last updated August 20, 2020.
https://melanoma.org/patients-caregivers/cutaneous-melanoma/
- National Human Genome Research Institute. Epigenomics Fact Sheet. Last updated August 16, 2020. https://www.genome.gov/about-genomics/fact-sheets/Epigenomics-Fact-Sheet
This slide show provides an overview of
genetic changes or cellular mutations in moles of the
skin which can help determine the best
melanoma treatments for each patient. A genetic mutation in these cells due to excess sunlight, or family inherited genes results in increased risk for the development of melanoma. Melanoma mutations promote cancer by helping cells stay alive, grow, and divide; they occur in high levels in tumor cells. A pigmented lesion assay (PLA) adhesion patch test can help diagnose melanoma at a very early stage. It is important to talk with your doctor about whether
genetic testing for melanoma risk is right for you.
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about melanoma which will help other patients, caregivers, and families.